It has often been said that "nothing in biology makes sense except in light of evolution." Evolutionary medicine is an attempt to apply this idea to the understanding and treatment of disease.
One of its goals is to provide “ultimate” explanations for disease as opposed to merely “proximate” explanations. This is the difference between understanding why disease happens versus just how. These two kinds of explanations are not opposing but complementary. Here's an example to illustrate, looking at different ways to explain the presence of symptoms like coughing, sneezing, fever, nausea, or diarrhea.
A proximate analysis of how these events occur would identify the specific pathogens, the sites of infection, and the specific physiological mechanisms that create cause/effect relationships between the infection and the symptoms. These topics form the bulk of medical education. In other words, the kinds of topics taught in medical school.
The ultimate explanation for these symptoms is a bit different and requires some knowledge about evolutionary biology. It asks why would the body have evolved to react to an infection by coughing, sneezing, or having a fever? The answer must explain why those symptoms would have increased reproductive fitness in our ancestors. Here, the apparent answer is that each of the above symptoms is a useful defense against infection. Coughing, sneezing, nausea, and diarrhea are all attempts to expel the pathogen from the body, and fever is an attempt to kill it with heat. This perspective helps clarify that coughing is not an illness, it is an attempt to defend against illness. This has implications for treatment.
We can make a similar analysis with regard to pain. Proximate explanations identify specific areas of tissue damage, and the physiological mechanisms that create pain, such as inflammation, nociception, central sensitization, or the activation of the limbic system in the brain.
The ultimate explanation for pain asks: why would the body respond to tissue damage with an unpleasant feeling? The answer is that pain defends the body against injury by motivating protective actions. Some evidence for this conclusion is summarized in a quote from a paper called An evolutionary medicine perspective on pain and its disorders:
The adaptive value of pain is demonstrated, often tragically, by syndromes of pain deficiency. People born with no capacity for experiencing pain accumulate increasing tissue damage, especially to their skin and joints, and they fail to get full defence against diseases and trauma. The result is deformity, mobility problems, and early death. …
Acquired syndromes of pain deficiency provided further evidence for the value of pain. Patients with syphilis get Charcot's joints because the destruction of pain pathways decreases normal small movements that protect cartilage and bone. Patients with leprosy lose peripheral pain and sensitivity to the extent that smoking cigarettes can result in loss of flesh down to the bone. Patients with central spinal cord lesions likewise experience flesh damage because of insufficient pain.
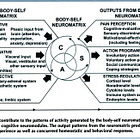
Thus, pain is a defense mechanism, just like coughing, sneezing, nausea, inflammation, and fever. This fact is essential to making sense of the incredibly detailed and complicated physiological evidence. It also makes it easier to organize your thinking about how to treat pain. The “ultimate” answer as to why any intervention is effective is that it reduces perception of threat, whether that is achieved through changing movement, posture, biomechanics, cognition, emotion, or the social environment.
Emotional pains
The evolutionary perspective helps us understand the link between pain, anxiety, and depression. Anxiety and depression are sometimes called “emotional pains” and function as defense mechanisms encouraging avoidance of threats. What threats?
Many common forms of anxiety involve circumstances that would've been dangerous to our ancestors, such as heights, snakes, infection, and the loss of social relationships. When these threats are detected, there are physical changes like increased heart rate, elevated blood sugar, and sweating. The mind becomes highly focused on the potential threat to the exclusion of other concerns. The adaptive value of these reactions are obvious - they divert your physical and cognitive resources towards dealing with danger.
The adaptive value of depression is a little harder to understand, but may involve an attempt to conserve energy and resources in times of stress, loss, or social defeat. It can prompt individuals to withdraw from unproductive or dangerous goals and reassess their strategies.
Consider the physiological response of a young male chimp to losing a physical contest for dominance with another young male. He immediately experiences a drop in testosterone. This is his body’s way of saying that continuing to fight for higher position on the status hierarchy is too dangerous, and to adopt a different strategy. He has low mood and energy for a while, but eventually comes to accept his lowered status. It’s exactly how the average sports fan feels after watching their team lose a big game. Depression is a natural response to loss, and encourages the abandonment of unreachable goals. We should therefore see depression as an adaptive response to losing something of value, such as a relationship or job. It could be helpful in encouraging beneficial changes in resource allocation, provided that the depression is temporary and/or proportional to the loss.
This raises an important question: Why are defensive mechanisms like depression, anxiety, and pain often set off by minor threats, and/or persist long after the threat has passed? Wouldn't natural selection have fine-tuned these protective systems to prevent them from becoming overactive and chronic?
One answer to this puzzle is that overprotection can be the best strategy if the consequences of failing to detect and defend against a threat are catastrophic. Smoke alarms are designed to be sensitive enough that false alarms are expected. This is because the cost of failing to respond to a fire could be extreme, while the cost of a false alarm is relatively minimal. Similarly, natural selection may have favored defensive systems that are easily triggered, even by innocuous stimuli. In other words, better safe than sorry.
Another potential evolutionary explanation for high rates of pain, anxiety and depression is that our bodies have somehow become dysregulated by the modern environment. This is the idea of evolutionary mismatch, which is a very good ultimate explanation for the high prevalence of obesity, diabetes, heart disease, and tooth decay in modern societies. These diseases are almost non-existent among hunter-gatherers. Does a similar logic apply to depression, anxiety and chronic pain?
It seems like a plausible theory. There are many facets of modern life that might get our defensive systems overactive, like sedentary lifestyles, long periods sitting at desks and in traffic jams, social isolation, bad diets, and constant exposure to bad news in the media.
I have previously talked about research looking at rates of chronic pain in hunter-gatherer populations. The quality of the evidence base is not that good, but it seems to show that chronic pain is actually common in communities living in ancestral conditions. Perhaps mismatch is not a good explanation for chronic pain in the modern world, and we just need to accept that many pains are a natural part of life.
Perhaps the better ultimate explanation for high rates of chronic pain involves the concept of trade-offs. This is the idea that almost any adaptation conferring some benefit will also exact a cost. For example, animals who adapt to become bigger and stronger will be better able to fight and defend themselves, but it will be harder for them to acquire the calories needed for survival. If an animal adapts to have a thicker fur coat, it will be warmer in the winter, but hotter in the summer.
When human ancestors stood up and started walking around on two legs, this freed their hands to perform a wide variety of useful tasks. But it also increased mechanical stress on the low back. Many evolutionary biologists point to this trade-off as a good explanation for the high rates of back pain in human beings.
The sensitivity levels and adaptive properties of the physiological systems that protect us also necessarily involve trade-offs. If the immune system gets more active it will get better at killing infections, but it all also make us sick more often and increase the risk for auto-immune diseases. A pain system that can modulate its sensitivity level (increasing sensitivity after an injury, and then returning to baseline after healing) provides a great benefit in fine-tuning the sensitivity to meet the circumstances. But it also runs the risk of getting “stuck” in the sensitized position if the system becomes dysregulated or confused in how it processes information related to threat. Same thing with depression - it is a useful adaptation when temporary, but if positive feedback loops cause someone to get “stuck” in the depressed state, this is a major cost.
Perhaps it is simply hard to design an intelligent system that isn’t prone to making some big mistakes. This is the current dilemma with artificial intelligence. Evolutionary medicine emphasizes the fact that natural selection is powerful in creating good designs, but certainly not all-powerful. Many of its designs remain prone to malfunction.
Aging is another ultimate explanation for disease. Natural selection works primarily by improving survival and reproduction in youth and mid-life when most reproduction occurs. There is less selective pressure against harmful genes that don't exert their effects until late in life.
Conclusion
So what are the main takeaways here? I think getting a basic understanding of the evolutionary perspective on pain helps make sense of all of the “how” information about physiology. It also points to the common features of any treatments that might be expected to reduce pain – they must all somehow serve to reduce the activity of the protective systems in the body.
This perspective also serves to clarify some of the confusion surrounding natural or “paleo” approaches to health and exercise. Advocates for these methods make some good points about the potential benefits of minimizing mismatches between the modern world and the ancestral environment. However, we have limited knowledge of exactly which differences between these two worlds are most important. Further, the evolutionary perspective makes clear that many forms of disease are indeed quite natural, even when the environment is optimized. Therefore, living like a caveman cannot be a cure-all.
Please note that this article only scratches the surface of this complex topic. For more information, check out some of the resources in references listed below, especially the books, articles, and podcasts by Randolph Nesse.
Related posts
References and Resources
Nesse 2019. An evolutionary medicine perspective on pain and its disorders Phil. Trans. R. Soc. B37420190288 http://doi.org/10.1098/rstb.2019.0288
Carl T. Bergstrom, Frazer Meacham, Depression and anxiety: maladaptive byproducts of adaptive mechanisms, Evolution, Medicine, and Public Health, Volume 2016, Issue 1, January 2016, Pages 214–218, https://doi.org/10.1093/emph/eow019
Büchel, Christian*. Pain persistence and the pain modulatory system: an evolutionary mismatch perspective. PAIN 163(7):p 1274-1276, July 2022. | DOI: 10.1097/j.pain.0000000000002522
Williams ACC. What can evolutionary theory tell us about chronic pain? Pain. 2016 Apr;157(4):788-790. doi: 10.1097/j.pain.0000000000000464. PMID: 26683235.
Walters Edgar T. and Williams Amanda C. de C. 2019. Evolution of mechanisms and behaviour important for pain. Phil. Trans. R. Soc. B37420190275 http://doi.org/10.1098/rstb.2019.027
Eric R. Castillo, Daniel E. Lieberman, Lower back pain, Evolution, Medicine, and Public Health, Volume 2015, Issue 1, 2015, Pages 2–3, https://doi.org/10.1093/emph/eou034
Plomp KA, Viðarsdóttir US, Weston DA, Dobney K, Collard M. The ancestral shape hypothesis: an evolutionary explanation for the occurrence of intervertebral disc herniation in humans. BMC Evol Biol. 2015 Apr 27;15:68. doi: 10.1186/s12862-015-0336-y. PMID: 25927934; PMCID: PMC4410577.
Good Reasons for Bad Feelings, by Randolph Nesse
Why We Get Sick, the New Science of Darwinian Medicine, by Randolph Nesse George Williams
Article by Randolph Nesse on Why We Get Sick
Good podcast with Randolph Nesse
The Story of the Human Body: Evolution, Health and Disease by Daniel Lieberman






I haven't read a single email newsletter from you that I haven't thoroughly enjoyed, Todd!
I was introduced to your work through 'Playing with Movement,' which I cited in my college psych thesis — and it's a joy to see how your writing continues to be insightful, thought provoking, and lucid. Kudos!
I agree, this framework is essential
I loved this interview of an evolutionary psychiatrist, you may find it interesting:
https://80000hours.org/podcast/episodes/randy-nesse-evolutionary-medicine-psychiatry/?utm_campaign=podcast__randy-nesse