Chronic Pain and Changes in the Brain
Low back pain is extremely common. In fact, if you don’t have at least some back pain every year or so, you’re kind of abnormal. (Not that you’re really missing out on anything.)
Fortunately, if you do get back pain, your chances of getting rid of it in fairly short order are excellent. More than 90% of acute back pain resolves on its own in just a few weeks or months without any specific intervention. But for some people, pain becomes chronic, lasting for years. Why does the course of back pain differ so much between different people?
The answer probably cannot be found by looking solely at the back itself. Experts have tried for years to explain back pain outcomes in reference to the results of physical examinations. But collecting evidence about posture, core strength, or the condition of vertebrae and discs does very little to help you make good predictions. Posture and MRI results correlate poorly with pain, and a single structural/physical cause for back pain is rarely found.
More recently, there has been more emphasis on subjective factors – pain intensity, negative mood, catastrophizing, depression, or job satisfaction. Accounting for these factors will help you predict back pain outcomes quite a bit better than just looking at the physical condition of the back. But a good deal of mystery would remain.
Some recent research from the lab of Vania Apkarian has led some very smart people to wonder whether he has discovered the “Holy Grail” of explaining pain – the precise factors that cause some people to develop chronic pain and others to recover.
If Apkarian is right, the grail is in the brain. (An important reminder and caveat: even when the brain is a major player in pain, this does not imply that pain is "in your head", that pain is your fault, that you can just think pain away, or that the body doesn't matter.)
Following is a collection of quotes from several papers from Apkarian’s lab. (See the bottom of the post for cites. Full text for each is available free online.) These help summarize the results and interpretations of his very interesting research, which mostly involves scanning the brains of people with and without back pain, and at various stages of recovery or chronicity.
The relationship between nociception, acute pain, movement and emotion
Pain is a conscious subjective experience that is most commonly driven by nociceptive activity. …
Conscious acute pain perception is highly malleable … pain perception can reflect moment-to-moment shifts in value judgments. …
The emotional limbic brain plays a critical role in bridging nociception and pain perception. …
[N]ociceptors can be active in the absence of pain perception . . .The primary reason I fidget in my chair while writing this article is because nociceptors innervating my skin, muscle, and bone command that my posture needs adjustment. …
The nociceptive control of behavior routinely occurs in the absence of consciously perceived pain, rendering it “subconscious.” …
Daily motor movements could easily produce injury and tissue damage if one exceeds their natural range of motion . . . which supports the conclusion that motor behaviors are collectively inhibited by nociceptors. …
We argue that nociception continuously occurs in the absence of pain perception and it is a fundamental physiological process . . . we presume that behaviors modulated by nociception, in the absence of pain, are contingent on already established habitual repertoires. In contrast, when pain is evoked it gives rise to new peripheral and spinal cord nociceptive learning/ sensitization, as well as emotional learning that is potentiated by the salience and perceived value of the aversive event.
Baliki 2015.
The Transition from Acute to Chronic Pain
[O]nly a fraction of subjects who experience an acute painful injury develop chronic pain
Hashmi 2013.
The majority (>90%) of individuals with acute low back pain recover full function in days or weeks with little or no lingering pain
Apkarian 2009.
The 2 critical questions that the field has yet to address regarding chronic pain are 1) Who is vulnerable to developing it? and 2) What underlies this vulnerability?
Hashmi 2013.
Earlier clinical studies have identified a long list of risks for chronic pain, such as demographics, affective states, lifestyle, comorbidities, and others, yet collectively such parameters account for a relatively small amount of variance for chronic pain (10% to 20%). In contrast, the brain’s anatomic and functional properties predict development of chronic pain at 80% to 100% accuracy.
Hashmi 2013.
Ample evidence now shows that the anatomy and physiology of the brain in chronic pain is distinct from that of healthy subjects experiencing acute pain.
Vachon-Presseau 2016.
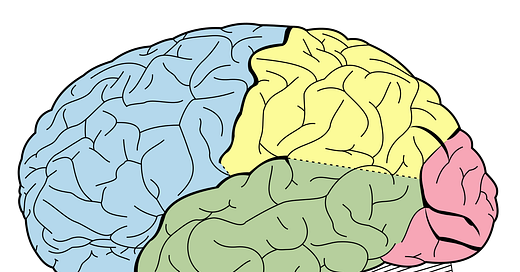
An accumulating body of animal and human literature has identified thecortico-limbic system, which is central to reward and motivated behavior, as a modulator for acute pain and as a mediator for chronic pain.
Vachon-Presseau 2016.
In a longitudinal brain-imaging study, individuals who developed an intense back pain episode were followed over a 1-year period, during which pain and brain parameters were collected repeatedly. At the time of entry into the study, strength of synchrony between the medial prefrontal cortex and nucleus accumbens (i.e. functional connectivity) was predictive (>80% accuracy) of individuals who subsequently transition to chronicity 1 year later.
Apkarian 2016.
Persistently enhanced functional connectivity between the mPFC and NAc may be interpreted as an increased emotional salience signal.
Vachon-Presseau 2016.
There is now good evidence that all components of the corticolimbic system are either affected by or control or amplify persistent pain states.
Vachon-Presseau 2016.
Redefining chronic pain
The definition of chronic pain remains tautological, as it simply asserts that it is a long-lasting pain, or a pain persisting past the normal healing period. …
We propose a novel definition of chronic pain. Rather than defining pain by its sensations, we propose a definition that emphasizes the neurobiological mechanisms that control behavioral adaptations, and we hypothesize that persistence of pain is likely mediated through the reorganization of the cortex by corticolimbic learning mechanisms. …
Long-term shifts in the threshold mechanisms that gate the conversion from nociception to pain also underlie the transition to chronic pain. We further propose that the threshold shift is dependent on limbic circuitry invoking synaptic learning-based reorganization. Taken together, these ideas can be simplified as a lowered mesolimbic threshold for the conscious perception of pain, which functionally renders the brain addicted to pain.
Baliki 2015.
The connection between chronic pain and negative mood
Just as nociception and pain protect against bodily injury by limiting behavior, negative moods minimize exposure to danger and promote survival by inhibiting behavior as well. …
Just as chronic pain conditions are associated with decreased hippocampal volume, a rich parallel literature indicates that depression is associated with hippocampal volume decrease. …
It is therefore not surprising that these conditions are often comorbid, and indeed, there is now a small but emerging literature regarding the interaction between negative moods and acute and chronic pain.
Baliki 2015.
Implications and new questions
How does this research add to what we already know? We have known for a while that chronic pain involves central sensitization and brain changes. But it was still possible that those changes were driven by persistent peripheral input. Apkarian's research seems to suggest that peripheral nociception is not the central driver of chronic pain.
It should be noted that some of Apkarian's research needs to be replicated, and that others may interpret his findings differently.
Apkarian is a featured speaker at the upcoming San Diego Pain Summit, which I will be attending in a few weeks (and so should you if you have read this far in the post.) I spoke there a few years ago and wrote about my experience attending here.
I will be sure to ask Apkarian some questions which are basically unanswered in his various papers: if chronic pain is mostly about the brain's emotional systems, what can we do, as a practical matter, to help treat or prevent it? And for people who do recover from chronic pain (like me and many others), how did their brains change? Did they revert or evolve?
I suspect there are no simple answers that apply to everyone, and that success for any particular person involves somehow changing the way their brain subconsciously connects movement, threat perception, and a sense of value or meaning.
Related Posts
I spoke with Dr. Melissa Farmer, one of the scientists from Apkarian’s lab in early 2021.
Resources/Citations
Apkarian, A Vania, Marwan N Baliki, and Melissa A Farmer. 2016. “Predicting Transition to Chronic Pain” 26 (4): 360–67. doi:10.1097/WCO.0b013e32836336ad
Hashmi, Javeria A., Marwan N. Baliki, Lejian Huang, Alex T. Baria, Souraya Torbey, Kristina M. Hermann, Thomas J. Schnitzer, and A. Vania Apkarian. 2013. “Shape Shifting Pain: Chronification of Back Pain Shifts Brain Representation from Nociceptive to Emotional Circuits.” Brain 136 (9): 2751–68. doi:10.1093/brain/awt211.
Vachon-Presseau, E, M V Centeno, W Ren, S E Berger, P Tétreault, M Ghantous, A Baria, et al. 2016. “The Emotional Brain as a Predictor and Amplifier of Chronic Pain.” Journal of Dental Research 95 (6). International Association for Dental Research: 605–12. doi:10.1177/0022034516638027.
Baliki, Marwan N, and A Vania Apkarian. 2016. “Nociception, Pain, Negative Moods and Behavior Selection” 87 (3): 474–91. doi:10.1016/j.neuron.2015.06.005.Nociception.
Apkarian, A.V., Balik, M.N., Geha, P.Y. 2009. “Towards a Theory of Chronic Pain.” Progress in Neurobiology 87 (2): 81–97. doi:10.1016/j.pneurobio.2008.09.018.Towards.